GUEST BLOGGER: Kathryn Biel
As a physical therapist, and a pediatric one at that, I get numerous referrals every year for children who toe walk. Often, that is the only information provided from the physician. Early on, I would look at these children and think, “Where to start?”
As with most cases, a good history is critical. Does the birth history suggest a neurological insult? Is there a history of autism or sensory processing disorder? Is there a structural deficit?
Following the history, evaluation is next. What is the range of motion and muscle tone?
When the child has a diagnosis of cerebral palsy, the treatment path is generally straight forward, including tone management, range of motion, and bracing. However, when there is no diagnosis, things are trickier. And this is where I used to get stuck. Especially if the range of motion and muscle tone were within normal limits. With some children, it’s easy to see that toe walking is a result of sensory-seeking. Walking on the toes provides increased proprioceptive input through the leg joints, thereby giving more feedback about the child’s position in space and his or her relationship to the floor. Sometimes, toe walking is the result of sensory avoidance, as the walker does not like input on the bottom of his or her foot.
Those are the “easier” sensory things to tease out. What about the children who are intermittent toe walkers? Or those who are not apparently sensory seeking or avoiding? Another aspect to consider is the integration of primitive reflexes. Children with unintegrated primitive reflexes, especially the tonic labyrithine reflex, can demonstrate toe walking as a sign. The retention of reflexes can also indicate an immature or neurological system that is under stress. The stress can activate the sympathetic nervous system, making the child function in a “fight or flight” state. A primary sign of the fight or flight state of arousal is toe walking. Other signs of this heightened state of arousal is increased respiration, decreased attention, increased visual scanning, and agitation.
Also, in the absence of sensory issues, a suggestive birth history, or a diagnosis of cerebral palsy, other neuromuscular disorders (Muscular Dystrophies, even in females) should be considered. This is especially important to follow through with when treatment does not change the toe walking, muscle length or muscle tone.
*********
Why is it important to address toe walking? An equinus gait is energy-costly, as it causes the ankle and knee joints to lock out, thereby preventing the transfer of energy in the form of momentum through the legs. The forward movement of the body that is normally achieved by a heel-toe gait is absent. Additionally, toe walking causes compensatory strategies throughout the rest of the body that can lead to long term imbalances and eventually pain and dysfunction.
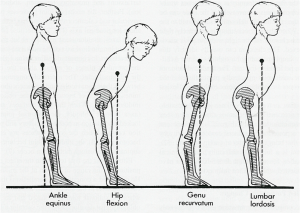
These postural compensations will impact lower extremity muscle length, posture, core stability, and vision. The postural implications can also play a role in scapular and shoulder function, thus setting the child up for a life time of dysfunction.
What challenges are you finding with your toe walkers? Are you getting referrals for toe walking? How are you treating it?
~Kathryn Biel, PT, DPT
]]>
