
Feeding difficulties in children — particularly those intertwined with sensory processing — come with a few hurdles. For example, parents might find encouraging their children to eat nutritious foods challenging.
Children with sensory processing disorders might avoid certain textures, such as mushy foods like mashed potatoes or foods at specific temperatures, like hot soup.
Understanding and addressing these sensory processing and feeding issues requires a unified approach of specialized insights by occupational therapists, nutritionists, educators and parents.
What Are Sensory Processing Disorders?
Sensory processing disorder (SPD) influences how the brain handles sensory information. SPD impacts what we see, hear, smell, taste or touch. Some may be overly sensitive, while others require more stimuli to notice things. This disorder is not limited to children. Often times, adults with SPD have found ways to adapt and cope by creating a good fit between their daily life and their unique sensory preferences and needs.
SPD has three main patterns, which include the following:
- Sensory modulation disorder (SMD): SMD involves difficulties regulating responses to stimuli. Individuals can either be over- or under-responsive or have sensory cravings. With SMD, kids might feel distress around textures, avoid bright lights or seek sensory experiences in unique ways.
- Sensory-based motor disorder (SBMD): SBMD involves balance, coordination and motor tasks. This may be related to differences in vestibular, proprioceptive, kinesthetic and/or visual processing skills. A child with dyspraxia, for example, can find it challenging to translate sensory info from these systems into effective and efficient movements. An observer may see postural difficulties, loss of balance, or uncoordinated movements as the child moves throughout their environment.
- Sensory discrimination disorder (SDD): The SDD profile refers to how accurately one interprets sensory information. SDD has eight subtypes that align with the sensory systems; for example, tactile DD, vestibular DD and auditory DD, to name a few. Children with SDD struggle to understand the nuances of sensory stimuli for things, people and places.
The Connection Between Sensory Processing Disorders and Feeding Difficulties
SPDs may not be officially recognized as a standalone diagnosis, but their impact on how the brain processes sensory information is indisputable. A heightened sensitivity — or the lack thereof — often affects various aspects of daily life, including one’s eating habits.
The sensory experiences associated with food are crucial in the eating process. For those with SPD-related issues, these aspects can trigger numerous responses.
Imagine how sensory sensitivities influence appetite and hunger signals. Children may struggle to recognize hunger cues amidst a whirlwind of sensory information. It may lead to erratic eating patterns or refusal of certain foods based on their sensory characteristics. Some children might also take a rigid approach to food, sticking only to specific brands or variations of certain foods due to sensory comfort zones.
Extreme picky eating or Avoidant/Restrictive Food Intake Disorder (ARFID) may also manifest in children. Those with ARFID may exhibit various behaviors tied to sensory processing issues. They may avoid foods due to sensory characteristics or experience fear around trying new foods. This reluctance may lead to nutritional deficiencies and marked interference with psychosocial functioning.

Identifying Sensory-Related Feeding Challenges
As a therapist or educator, you play a crucial role in identifying these issues early. Here are some red flags and behaviors that might signal sensory-related feeding issues:
- Gag reflex: Children may gag at the sight, smell, touch or taste of certain foods. This reflex could stem from sensory sensitivities or underlying difficulties in chewing or swallowing.
- Texture preferences: This is a preference for only specific textures — such as crunchy or soft — and an insistence on specific brands, colors or flavors. It can include an avoidance of foods outside of the preferred texture. Children may demonstrate a “food jag” when they will only accept specific textures and types of food.
- Discomfort with messiness: Children may have avoidance or discomfort with messy hands or face. Be it during meals or in activities like crafting or playing in the sand. This raises the question of possible tactile sensitivity.
- Food pocketing: This includes individuals who excessively stuff their mouths or pocket food in their cheeks. Food pocketing may be due to poor coordination, poor sensory awareness in the mouth, and/or chewing difficulties.
- Lack of oral exploration: Infants and toddlers typically demonstrate oral exploration of items in their surroundings. Educators and therapists can offer safe and developmentally appropriate items and opportunities for mouthing and chewing. Without this exploration, infants and toddlers may show more difficulty as they learn to eat solid foods.
- Extended mouthing behaviors: While lack of oral exploration is often problematic for feeding development, extended mouthing behaviors past developmental expectations can also indicate sensory processing issues. Extended mouthing behaviors are when children continue to mouth and chew on various objects outside of typical developmental windows, such as chewing on clothing, pencils, or straws.
You can help parents or caregivers be aware of these signs. Early intervention can help by looking at sensory processing differences as one of the contributing factors around feeding difficulties and it can offer strategies to address them. These efforts can contribute positively to a child’s development and foster a positive relationship with food and eating.
Assessment Tools for Identifying Sensory-Related Feeding Challenges
As an early childhood educator or therapist, you can use formal assessment tools to help identify when sensory processing disorders may be contributing to sensory-related feeding problems. The following tools can help you understand a child’s unique sensory needs and challenges and therefore, develop effective intervention strategies:
- Sensory processing measure (SPM): This system of caregiver and teacher questionnaires assesses sensory processing abilities across different environments between home and school. It provides insights into sensory modulation, sensory discrimination and behavioral outcomes of sensory modulation.
- Sensory Profile-2: This questionnaire has forms to be completed by caregiver, adolescent self-report, and/or teacher to help identify an individual’s sensory processing patterns and preferences. Results are grouped into summary quadrants to shine some light on a child’s pattern of responses and sensory-motor needs in everyday situations — including mealtimes.
- Pediatric eating assessment tool (PEDI-EAT): This is a tool specifically designed to assess feeding difficulties. It evaluates mealtime behaviors, oral-motor skills and functional eating skills.
- Clinical observations: Skilled observation during mealtime or multi-sensory activities can provide insights into a child’s real-time responses to sensory stimulation.
- Structured interviews and caregiver reports: Engage parents or caregivers through interviews or questionnaires that consider all types of sensory stimuli and their child’s typical responses. Gather information about typical mealtimes, including the food and drinks offered, mealtime partners, and the physical environment. The answers can help you gather detailed information about a child’s feeding skills and the impact of sensory differences or challenges on their participation with feeding and eating.
- Multidisciplinary evaluations: Collaborative assessments with other specialists such as speech language pathologists, occupational therapists, nutritionists, and developmental pediatricians can offer a holistic view of the child’s abilities and needs.
5 Strategies to Create a Sensory-Supportive Eating Environment
As a therapist or educator, you can help parents or caregivers try different strategies to create a sensory-supportive eating environment for the child and family. These approaches aim to promote a positive relationship between children and food, minimize stress and enhance nutritional intake.
1. Sensory-Friendly Meal Environments
Establish structured and consistent settings that offer predictability and minimal distractions for attention during meals. Consider dimming the lighting, using music or calming background noise, and offering preferred seating to your child to promote comfort and calm. The more relaxed the child is, the more regulated they’ll be- and that promotes more engagement with food and eating.
2. Adaptive Feeding Tools
Adaptations can be made to heighten or lessen sensory stimuli, depending on what type of support the child needs. Experiment with different types of utensils and dishes and share with parents which ones worked best for their child. This might mean adapting utensils for more independent and accurate self-feeding, or using non-traditional utensils to add novelty and fun to the mealtime experience. Altering the presentation of the food by using small dishes or compartments versus one large serving plate or cutting board can also promote more curiosity and engagement in some hesitant eaters.
3. Interactive Food Activities
Demonstrate how to use interactive food activities to promote sensory exploration with texture, sights and smells. Show parents how you set up tactile sensory bins with various textures to encourage exploration. Know that it is okay to “play with your food” to learn more about how it feels, what it looks like, how it smells and how it tastes. Use kid-safe but grown-up looking tools and utensils to interact safely and creatively with new or familiar foods.
You can also offer strategies to involve kids in meal preparation. This changes cooking into a sensory-rich, low-pressure activity for them. Children may become more familiar with new foods while cooking in a relaxed environment. Washing, rinsing, drying, sorting, peeling, slicing, grating, opening, and more will teach cooking skills and offer safe exposures to new sensory experiences.
4. Personalized Food Selection and Preparation
Guide parents to encourage children to make choices, based on what’s appealing to them about different foods. Consider the color, size, texture, and smell and give words to describe those features in the items the child chooses. Compare their choices to similar foods that they’ve tasted previously or to newly offered foods to build their repertoire of food awareness.
Additionally, involve the child in making simple alterations to the food, like changing the shape, or using a dip or sauce, to help bridge the gap to trying new items.
5. Building a Sensory Rich Vocabulary
Build comfort with novel foods through play and exploration. Discover what a food looks like, smells like, sounds like when they take a bite or chew. Is it sour, sweet or strong tasting? Is it dry or wet? Is it crumbly, squishy, mushy, or sharp? Does the color change or stay the same? Is it cold, warm, hot? With increased language to describe and understand their likes and dislikes, children may become more comfortable and confident tasting new foods.
You could also suggest playful interactions with food. Encourage their children to touch or explore different foods. This helps children become more accustomed to diverse sensory experiences.
The Role of Multidisciplinary Collaboration
The collaborative efforts among a team of professionals can be crucial in managing feeding challenges.
Speech-language pathologists (SLPs) help evaluate oral motor skills and design strategies to ensure safe eating practices, particularly around chewing and swallowing. Occupational therapists (OTs) focus on sensory integration and being regulated to engage in mealtime, while nutritionists help create balanced diets and address nutritional deficiencies. Medical specialists rule out underlying health issues, psychologists tackle emotional and relational aspects and educators implement strategies in the school setting so their students are fed and able to learn.
All team members strive towards a comprehensive and effective approach to addressing a child’s sensory-related food difficulties. This unified approach provides families with multiple points of support to tailor effective interventions for more mealtime success.

Enhance Your Care Through Collaboration and Education
Enhance your career to help more patients with Education Resources, Inc. (ERI). We offer comprehensive professional development and resources in different professions. Be it physical or occupational therapy, speech language pathology, special education or nutrition and dietetics — we have courses for you!
Whether through live webinars, in-person classes or on-demand courses, our offerings infuse practicality and passion. Learn what a difference evidence-based courses and learning can make in your career and the lives of those you serve.
Contact us online today to learn more about the power of collaborative care and continuous learning through ERI.

 We are so excited to announce the release of
We are so excited to announce the release of 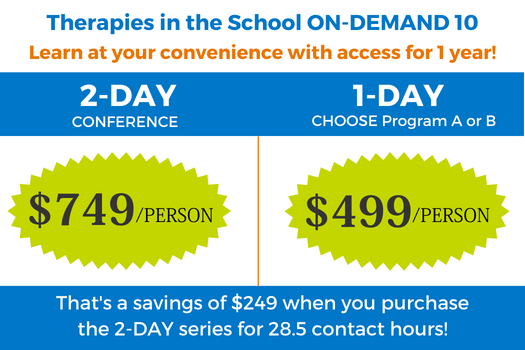 You can earn up to 28.5 CEU hours that appeal to different disciplines (PT, OT, SLP and special educators) and span many areas of practice. The sessions are equally geared towards experienced school-based providers as well as therapists new to this setting through engaging, evidence-based and practical content that can be put to work right away. There’s something for everyone!
You can earn up to 28.5 CEU hours that appeal to different disciplines (PT, OT, SLP and special educators) and span many areas of practice. The sessions are equally geared towards experienced school-based providers as well as therapists new to this setting through engaging, evidence-based and practical content that can be put to work right away. There’s something for everyone!

 ERI is excited to kick-off its inaugural
ERI is excited to kick-off its inaugural